The Ukraine-Russia war, launched by a Russian invasion in February 2022, has had devastating consequences for both sides, unprecedented in Europe since World War II. To highlight the scope, there are estimated to be over 75,000 Ukrainian amputees as a result of the war, over 40 times as many as U.S. Forces suffered during the entirety of the operations in Iraq and Afghanistan in the first decade of the new millennium. Although tragic by any metric, this also represents an opportunity to improve care for all victims of trauma-induced pain, with many of the greatest advancements in medicine such as antiseptic techniques, blood management, triage and evacuation strategies, and of course, postamputation pain and limb salvage strategies.
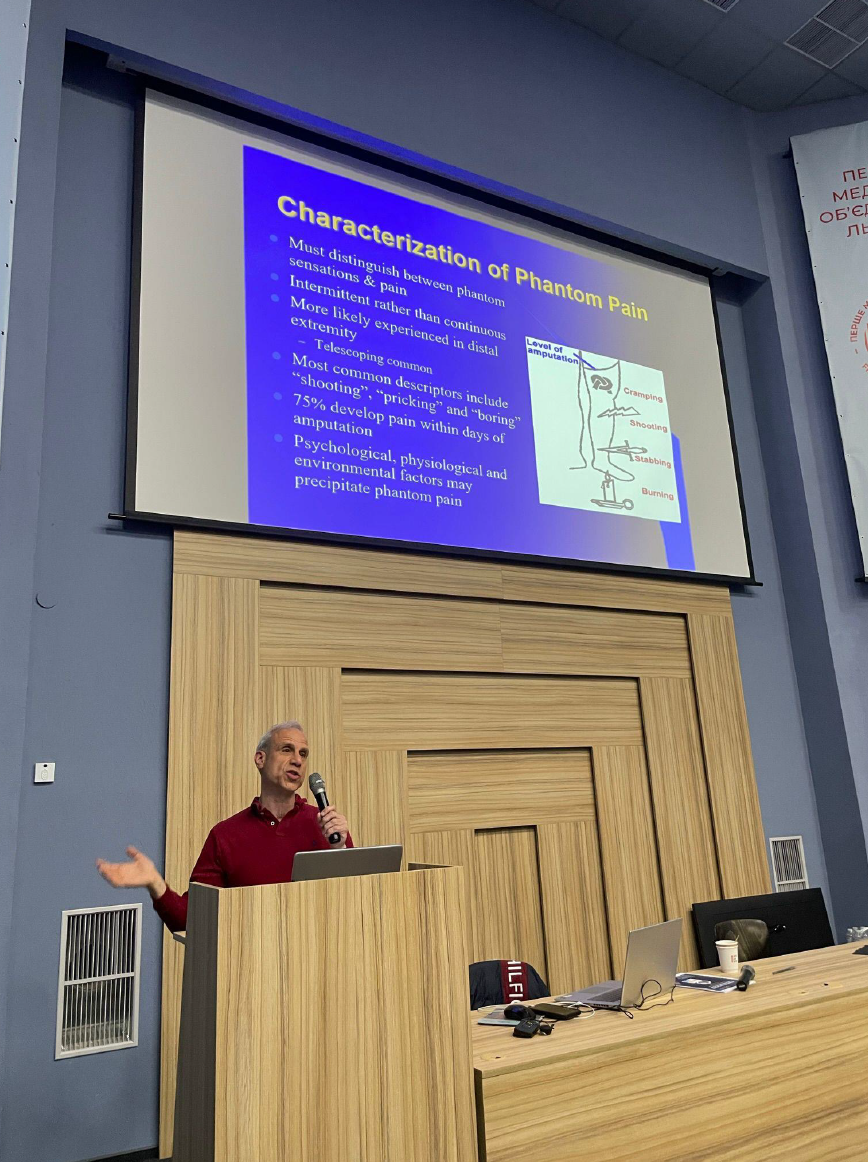
On April 26, sponsored by a host of organizations including ASPEN Medical, Alcoa, ESRA, ASRA-Pain Medicine, and AAPM, we hosted the largest medical conference in Ukraine since the war began. The focus was on acute and chronic pain medicine for battle-related injuries but also included talks on surgical advances, the organization of medical care during war, and basic pain concepts for a non-specialty audience. Although most practitioners cared for pain patients, there are no pain fellowships in Ukraine, no pain standards, and a wide divergence in how both acute and chronic pain are treated throughout the country.
More than 300 participants spanned the country, including anesthesiologists, neurologists, psychiatrists, surgeons, primary care doctors, and non-physician healthcare providers. We assembled an astounding array of speakers, all virtually, who hailed from South America, Asia, Europe, Israel, Canada, the U.S., and of course Ukraine, with the latter sharing their unique experiences and perspectives.
The Presidents of ASRA (Dr. David Provenzano) and AAPM (Dr. Charles Argoff) were among the people who generously donated their time to the conference. Outside of myself, all foreign speakers lectured virtually. There were 3 interpreters, with Ukrainian lectures translated into English and English lecturers translated into Ukrainian (the non-English foreign speakers gave their talks in English). There were several glitches along the way, including a 2-minute power outage that was quickly corrected during a talk from Jeeyoun Moon from Seoul National University, and a missile and drone attack on Friday, May 3rd that prevented my Ukrainian Co-Chair, Professor Dmytro Dmytriiev, from attending the weekend session he was slated to co-moderate. On the last day of the conference- Orthodox Easter- most attendees were virtual, with their videos showing several eating Easter Dinner. The after-action report will also note that there was a possible security breach on the last day during the Ukrainian speakers’, Dr. Andriy Khomenko, talk on minimally invasive ways to treat phantom limb pain, when outside information mysteriously appeared on the screen.
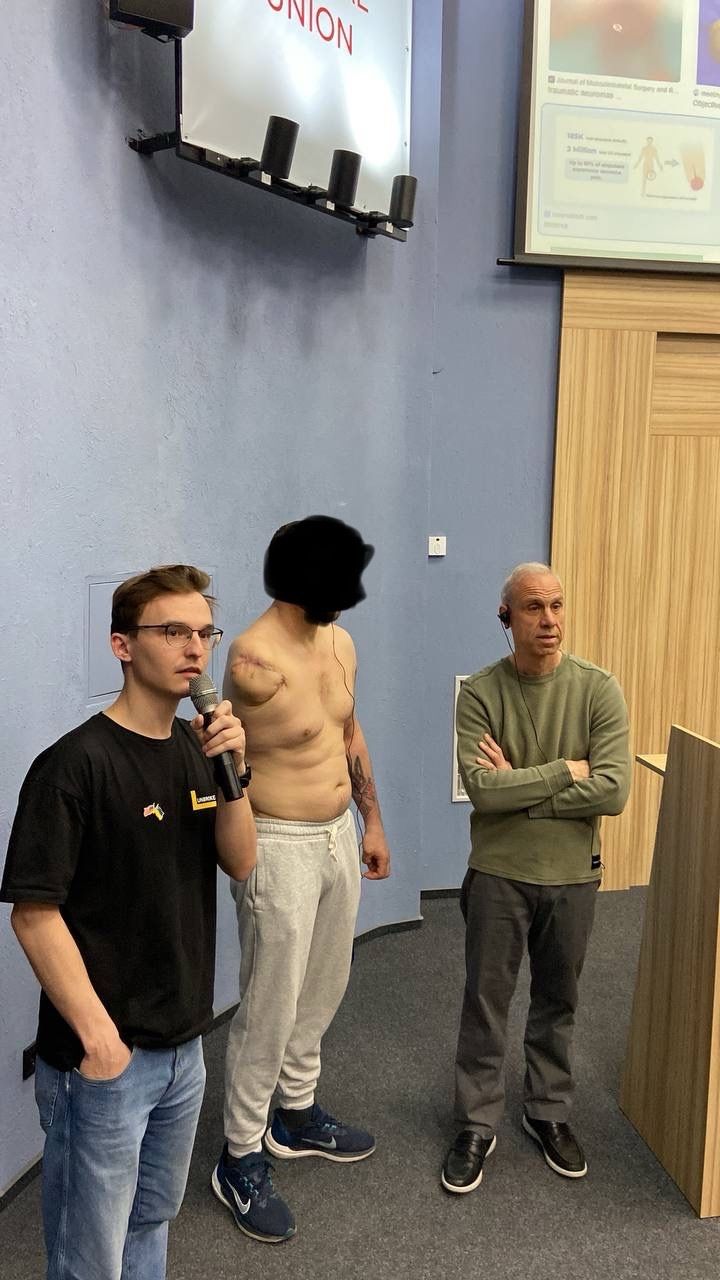
Before rounds, we did procedures in the operating theater. During martial law, the credentialing process for experts outside of Ukraine has been suspended, though I was there by invitation from the Executive Director of First Medical Union and UNBROKEN, Mariana Svirchuk. Throughout the conference, complex patients with polytrauma came into the auditorium where, as a team, we evaluated and recommended therapies. After the conference, a multidisciplinary group of physicians joined me in recommending treatment on some of the most refractory cases. This started with about 7 people on Monday but by Friday the number had ballooned to over 15. The days often ended after 9 PM.
There were air raid sirens most days, but we never felt unsafe. The last evening, we toured the war cemetery, where my colleague Dr. Roman Smolynets, who played an instrumental role in the day-to-day management of the conference, ran into the widow of someone he knew from school.
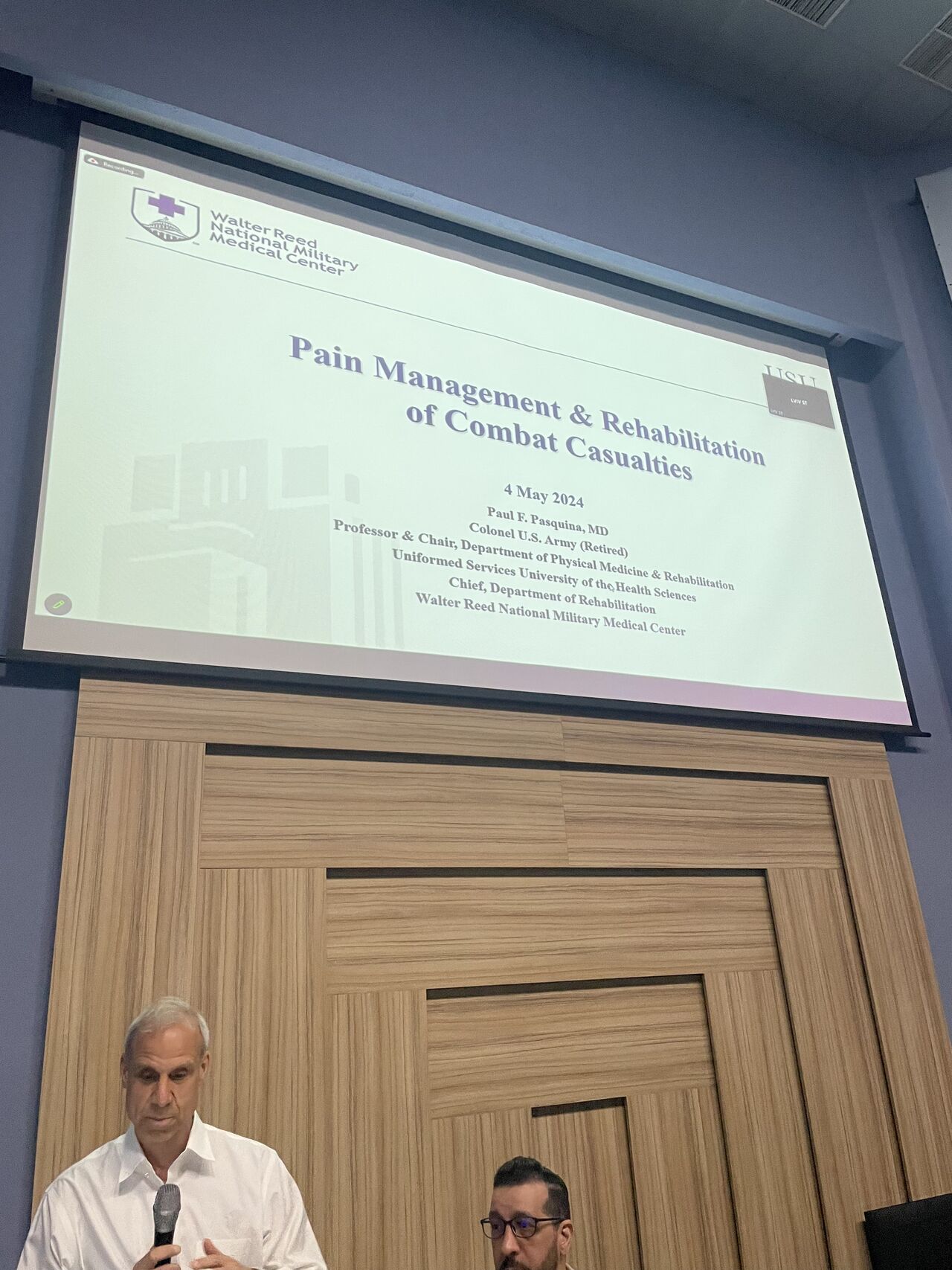
The conference was incredibly fulfilling, but this was not a one-and-done event. Our team from the Defense Health Agency, which includes Dr. Paul Pasquina and Terry Rauch Sr., intends for this to be the start of a sustained, mutually beneficial relationship. Spurred on by the 2024 National Defense Authorization Act, which mandates that the Department of Defense study novel treatments for PTSD, traumatic brain injury, and limb amputation, our intention is to expand our multi-center study. This includes evaluating stellate ganglion block and ketamine infusions for TBI and PTSD to include Ukrainian sites; funding and implementing a study evaluating peripheral therapies for phantom limb pain; setting up a multi-institutional pain database that can be used to evaluate therapies already being used to treat trauma-related pain; and continue to engaging in educational endeavors related to pain care and related topics.
Written by:
Steven Cohen, MD, Edmund I. Eger Professor of Anesthesiology and Vice Chair of Pain Medicine, Northwestern University Feinberg School of Medicine and Director of Pain Research, Walter Reed National Military Medical Center
Terry M. Rauch, PhD, Director, Defense Medical Research and Development Program, U.S. Department of Defense
Additional photos provided by:
Roman Smolynets, MD, an anesthesiologist and intensive care specialist at Lviv Emergency Hospital. During the war, he works at the hospital, helping evacuate victims from hostile sites